Table of Contents
Name of Procedure
Fluoroscopic/x-ray guided intercostal nerve block (ICNB)
Sample Opnote
Goal
To inject mediation around an intercostal nerve such as local anesthetic or steroid.
Indications
Pain mediated via the intercostal nerves such as pain from intercostal neuralgia, rib fractures, post surgical pain in the chest, upper abdomen (ie, thoracotomy, thoracostomy, mastectomy, gastrostomy, and cholecystectomy).
Contraindications
- Common contraindications
- Blood thinners – See ASRA based guidelines (and an abbreviated protocol) for managing various blood thinners pre and post procedure
- One functional lung on the side of the procedure might be a contraindication as pneumothorax on this side could be disastrous.
Anatomy
The ventral rami of spinal nerves T1-T12 form the intercostal nerves. A bit lateral to the foramen the nerve begins it’s path parallel/inferior to the rib along with a vein and artery:
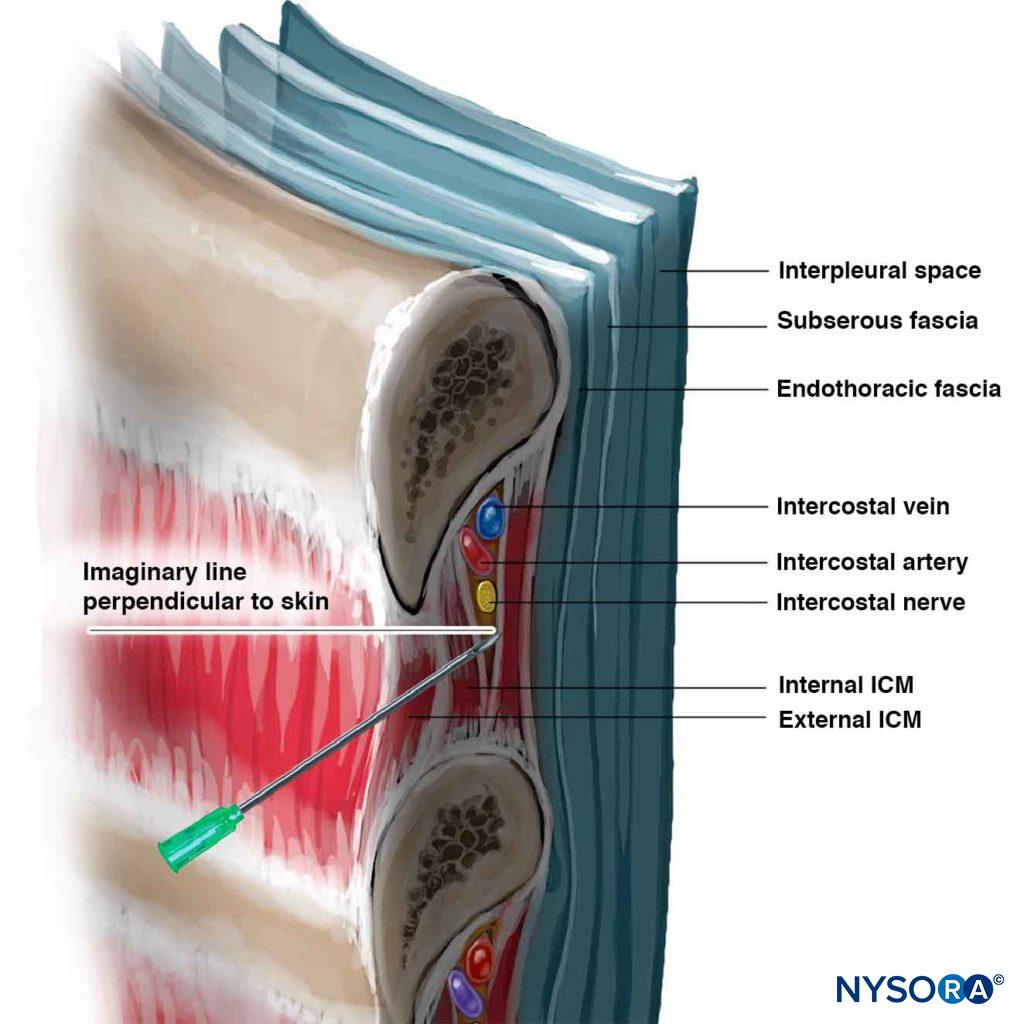
Anatomical variations, branches and details are nicely reviewed at the NYSORA link above. Some particularly relevant details:
- The average distance from the posterior rib to the pleura is 8mm, so very small adjustments are needed to avoid a pneumothorax
- a cephalad needle trajectory (as seen in the image) helps to get close to the nerve.
The nerves innervate the chest/abdominal wall according to typical dermatome patterns. Keep in mind that to cover a dermatome it might be necessary to block 1-2 levels above and below the dermatome due to variation in innervation.
Equipment/Skills/Setup
Core Equipment/Disposables: See our disposables/equipment article for “core” items that are common to all procedures.
Core Skills: See our guides to obtain images of the cervical, thoracic, or lumbar spine. Then steer a needle to direct it under the skin.
- Due to the close proximity to vascular structures, you can consider using a less particulate steroid (if injecting steroid) such as dexamethasone.
- The primary needle will be a simple 25g x 1.5″ hypodermic needle (in larger patients, a 22g x 3.5″ quincke needle)
Landmarks and Patient Positioning
Position the patient in a basic prone position so the C-arm can go under the patient at the level of the ribs/intercostal nerves that are being treated.
Technique
- Obtain an AP view with T12 in view.
- Use T12 to count up to the levels that you want to treat.
- Start at the bottom level that you want to treat so you can just walk your way up and stay oriented.
- You’ll enter skin:
- About 3-4 inches lateral to the midline
- About 1-2cm inferior to the inferior border of the target rib
- You’ll target to hit the posterior/inferior border of the rib
- By hitting bone, you will ensure that your needle is at a safe depth before the next steps
- By starting inferior to the rib you will have a cephalad needle trajectory
- Once you hit bone, simply walk off inferiorly and slowly.
- Once you feel the needle advance slightly you know that you are passing under the bone
- You should be entering the space with the nerve as shown in the diagram above.
- Experience will teach how much you can advance, but it isn’t much (<1cm in total)
- Inject contrast. You want to make sure that you don’t have vascular spread and should see contrast spread along the nerve distribution.
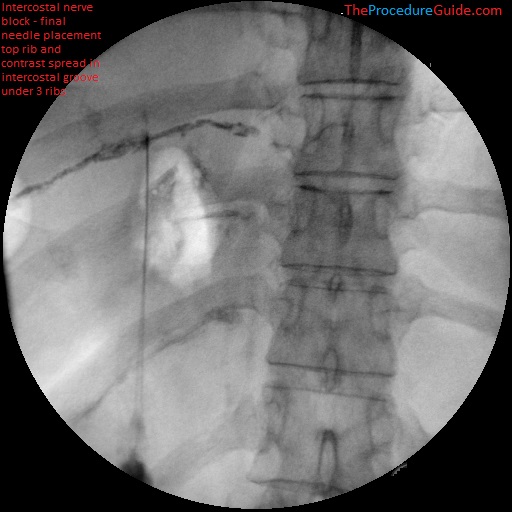
Fluoroscopic intercostal nerve block with contrast spread
- In the image above you see a cephalad direction, lateral of midline starting position, and good contrast spread.
- Repeat for any other levels
Tips
- Risk management:
- As noted above, pneumothorax is a possible complication. Because of the potentially severe consequences it might be good to watch the patient for an extended period of time, monitor vitals, and listen for breath sounds prior to discharge.
- Similarly, due to the close proximity to vasculature, vascular uptake rates could be high and depending on volume of anesthetic, could lead to systemic local anesthetic toxicity.
- Needle selection:
- In most cases a 1.5″ hypodermic needle is sufficiently long.
- This allows you to skip subcutaneous local anesthetic: just insert the 25g hypodermic needle directly down to rib.
- Because of the shallow depth, a straight needle (as opposed to a bent needle) might be fine (and might be easier since you want to walk off bone but want the needle to advance without curving too much after walking under the rib).
References
- Intercostal Nerve Block – NYSORA
- Excellent review of most of the topics above related this procedure, but the technique is focused on ultrasound guided procedures.
- Atlas of Pain Medicine Procedures – Chapter 57: Intercostal Nerve Block
- Another general overview
- Utility of Intercostal Nerve Conventional Thermal Radiofrequency Ablations in the Injured Worker after Blunt Trauma
- Good review of several cases that could benefit from intercostal nerve block (and even potentially ablation).
