Table of Contents
Name of Procedure
Ultrasound guided seldinger venous access
Sample Opnote
Goal
To percutaneously establish venous access with a catheter.
This article is focused just on obtaining access. Any procedures performed after access are discussed separately in their own articles. Likewise, choice of access sites, purpose of sites, variations between sites, etc are not reviewed in this article.
Indications
Any of a variety reasons that necessitate venous access:
- Central or peripheral venous access for blood sampling, monitoring, or medication administration (such as an internal jugular or femoral vein line)
- Access for minimally invasive procedures such as angiograms/venograms, embolizations, venous ablations, etc.
Contraindications
- Local skin infection at the access site
- Lymphedema or DVT
- Coagulopathy (relative contraindication)
Anatomy
Anatomy will vary greatly depending on which veins are being accessed.
Equipment/Skills/Setup
Oftentimes kits are available, depending on the specific procedure you are doing.
- In a kit, the access needle/trocar, wire, catheter and dilator will all be sized to match each other.
- If assembled separately you’ll need to ensure appropriate sizing.
Extra supplies in the kit can in fact make things confusing. So, for the actual seldinger access, make sure you have these basic items ready to grab with one hand:
- 3-5cc syringe with local anesthetic (lidocaine 1%) to anesthetize
- May want to avoid lidocaine with epinephrine as that could theoretically cause some vasospasm of the vein that you are trying to access.
- Access needle
- Wire
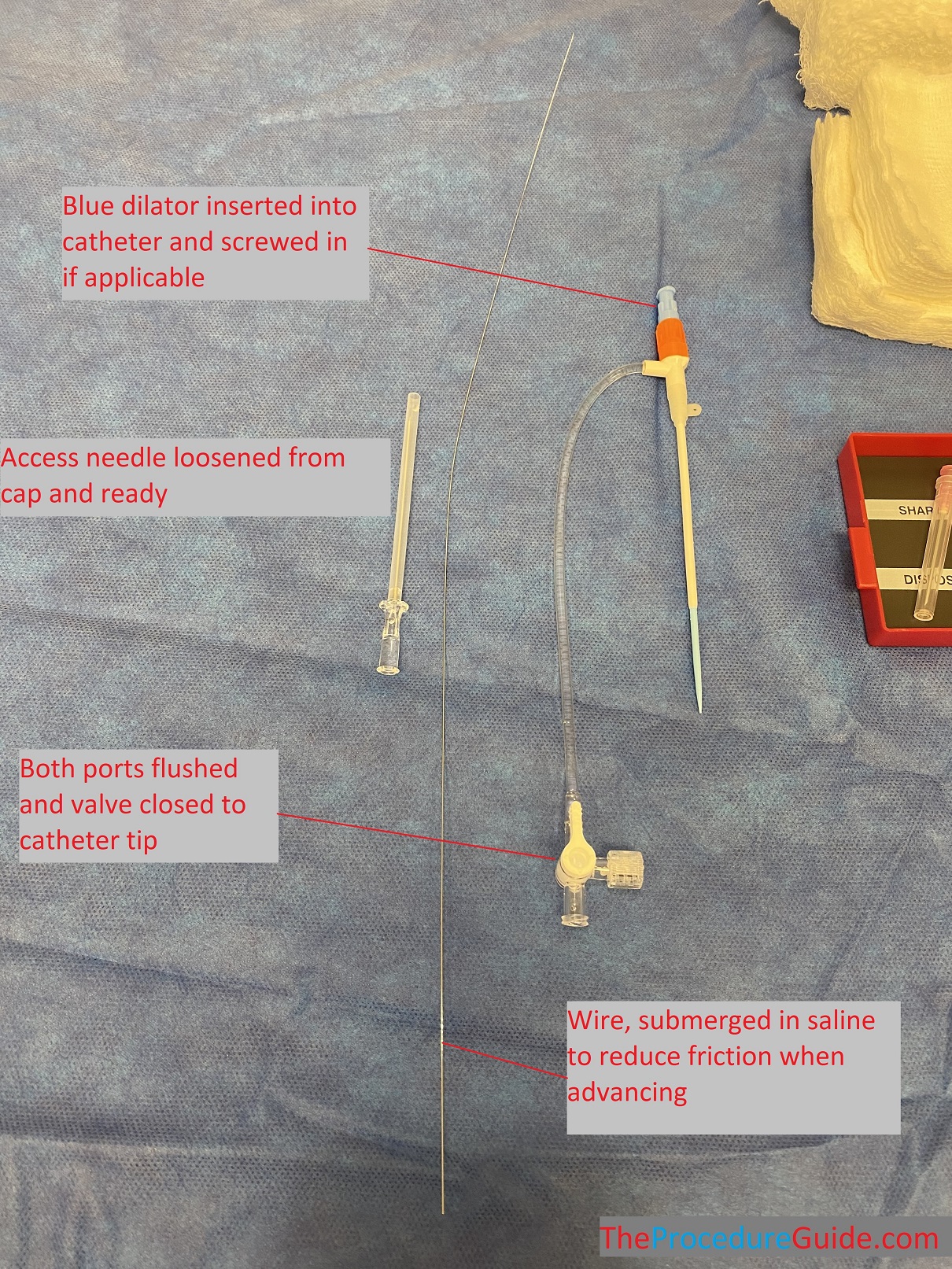
- Dilator and catheter (oftentimes designed to be assembled and inserted as one unit and then separated after it’s fully inserted)
- Flush saline through both ports
- Turn the valve so it’s closed towards the patient/catheter tip (so there’s no backflow after insertion)
- Have all items out of or loosened from their caps so you can easily grab them with one hand.
- Submerge the wire in saline to wet it and reduce resistance when advancing it.
- Ultrasound probe that’s draped with a sterile cover
Landmarks and Patient Positioning
Again this will vary greatly based on the specific procedure that you are performing. A few basics to keep in mind:
- For venous access specifically it’s helpful to drop the access area below the level of the heart to allow passive accumulation of blood and dilate the vein.
- Keep in mind the length of your catheter:
- You usually want to “hub” a catheter meaning the hub goes to the skin. Keep in mind the catheter length and how much travel (subcutaneous and intravascularly) that you need in order to accommodate that length.
- Keep in mind the vein path:
- If possible a straight vein with few branches and valves is ideal to advance the catheter.
- The wire can help get around this to some extent but it’s still good to choose a vein and entry point that makes it as easy as possible.
Technique
- Obtain an adequate view of the target vein’s access point.
- It can be accessed in a transverse or longitudinal view but we’ll focus on longitudinal access since it requires good control to keep your needle in plane and gives you a view of the entire process.
- Start by scanning in transverse, up and down from your access site to get a quick sense of the trajectory of the vein and it’s branches/valves.
- Rotate to a longitudinal view and orient the ultrasound probe so that the needle entry will be on the right of the screen.
- Ready for access (see image below):
- You will usually access with a needle angle of around 45 degrees
- Sometimes shallower if the vein is superficial
- Or sharper if the vein is deep
- Keep the target entry point on the vein in the middle or left 1/3rd of the ultrasound screen.
- This gives you space on the right to see your needle trajectory.
- Change the depth of the ultrasound image: you only need to see as deep as the deep wall of the vein.
- You will usually access with a needle angle of around 45 degrees
- Anesthetize
- Anesthetize the skin just proximal to the ultrasound probe.
- Advance the 25g needle and keep it in plane and watch on ultrasound to map out the trajectory that you will use with your access needle (and to anesthetize a track)

- Access the vein
- Remove the 25g and insert your main access needle, following the same track.
- Try to stay in-plane the entire way.
- Once the tip of the needle is at the vein wall there are several things to consider:
- Simply advancing may be enough to enter the vein.
- Sometimes veins “roll” and your needle will fall to one side of it.
- Some traction on the skin below or above the access point might help anchor it.
- Sometimes the needle itself can anchor the vein a bit: just apply pressure at the vein wall right before puncturing it with a slight stabbing motion.
- Changing your needle trajectory right at the vein wall to a more steep angle might help to puncture the vein and then you can flatten out the angle again after entry.

- Insert wire
- With the needle held still, insert your wire.
- In many cases you don’t need to follow the wire’s trajectory if you know the vein’s trajectory.
- If however there are branches you may need to steer your wire to your desired path.
- Remove the access needle
- With the needle held still, insert your wire.

- Insert the dilator/catheter combo over the wire.
- Before you push the dilator into the skin, feed wire back till you can grab it on the back of the dilator/catheter.
- Always ensure that you have hold of some wire when advancing over the wire.
- Hold the wire in one hand and advance the dilator/catheter combo with the other hand
- Expect some resistance at the skin and vessel
- Keep a good broad grip over the entire apparatus and apply most pressure right near the skiing to prevent sudden bending/kinking
- Pull the wire and dilator as one unit.
Tips
- Blind seldinger technique
- The steps above are basically the same for a blind approach. A few notes:
- You don’t know your needle placement when doing it blind, so you can attach a small syringe and apply negative pressure while advancing the needle to see if you enter the lumen.
- Learning the feel of different tissues is more important and will simply come with time.
- One or two person procedure
- If you have a second person to hold the probe that makes the procedure easier but it may often have to be done with one person:
- Before starting, make sure all supplies are laid out for easy one handed grab/use.
- Use your non-dominant hand to hold the probe still. Brace yourself well and use a light touch on the probe so that you can comfortably hold the probe in a stationary position for a while.
- Once your access needle is in place, just put your probe down, and hold the needle with your non-dominant hand. While holding, brace your palm on the patient to help ensure that the needle doesn’t exit the lumen.
- The steps above are basically the same for a blind approach. A few notes:
- Resistance
- If the wire has resistance it could be that:
- The wire is outside the lumen
- The wire is hitting the intraluminal wall while changing direction
- The wire is hitting thrombus
- The wire is dissecting the blood vessel
- Use your ultrasound probe to investigate.
- Once the wire and needle are in they will usually remain stable so that you can let go and grab the probe (but an extra set of hands can help here)
- If the wire has resistance it could be that:
- Pulling wire
- Pulling wire through a needle can theoretically shear/tear the wire, but usually it is ok as long as it pulls smoothly without resistance. If not, pull the needle and wire together.
- Passing “through and through.
- Sometimes it’s hard to penetrate a small vein without passing through the back/deep wall. This usually isn’t a problem unless there is a problematic structure deep to the deep wall.
- In this case just pull the needle back very slowly till the needle tips enters the lumen
- Ultrasound guidance can help here but this might be a case where imaging is suboptimal and it isn’t clear when you’re in the wall.
- Also look for blood return, but remember that a small venous vessel will bleed slowly. You should pull small amounts and allow time for blood return if using this technique.
References
- Seldinger Technique for Intravenous (IV) Line Placement
- Some illustrations and a procedure description for peripheral IV placement
- Seldinger technique
- Very good video of live IJ placement with some small amount of ultrasound guidance
- Practical guide for safe central venous catheterization and management 2017
- Thorough review of central venous access including detailed procedure descriptions and discussions on related peripheral issues such as complications, verification, issues specific to central lines, etc.
- Use of Ultrasound to Guide Vascular Access Procedures
- Comprehensive guide from the American Institute of Ultrasound in Medicine
- Thorough review of ultrasound use for venous and arterial access with the beginning sections focusing on basics, technique, and some images.
